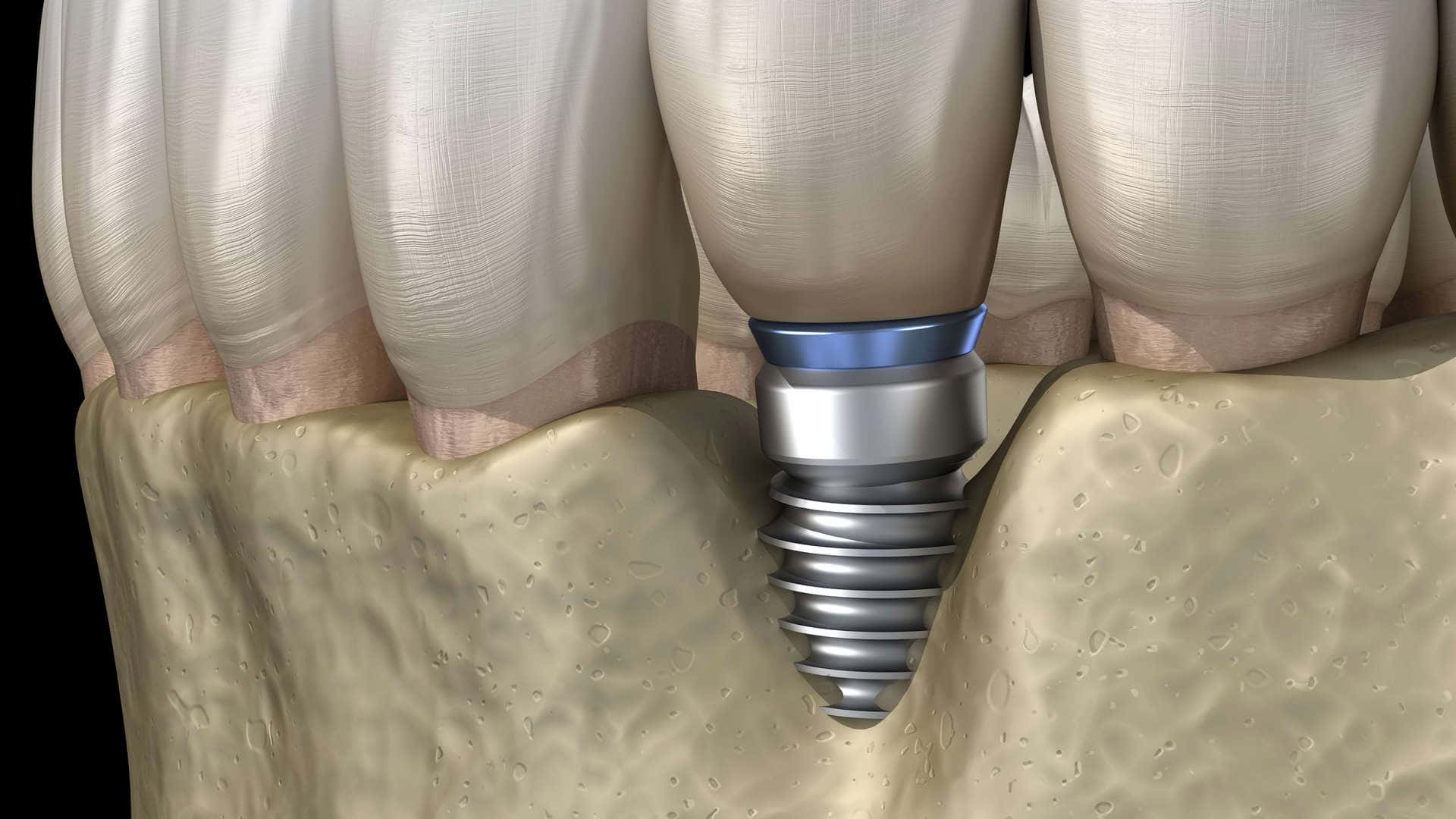
Dental implant failure is a rare occurrence, but that doesn’t mean there aren’t some problems, risks, and complications. Dental implants have a high success rate of more than 95% and last a lifetime, but some people experience failure in their implants. It is estimated that less than 5% of dental implants fail, either shortly after a procedure or months or even many years later.
Dental implant problems: what’s the worst that can happen?
If you are planning to have implants or if you currently have an implant, here’s what you need to know about the risk of implant failure and other potential complications.
While some problems can be avoided or prevented by the patient, some develop as a result of poor treatment planning by the dentist.
Although the risk of dental implant complications is extremely low, dental implants do not hurt like problems with our natural teeth and therefore our body does not alert us to any problem that may exist. In this article, we will share with you what can happen if you choose this type of dental procedure and something does not go smoothly.
Common dental implant problems
While there is a possibility of complications with dental implants, the majority of these can be managed if they are caught early and no major mistakes have been made in their design and surgical placement. Most of these occur during the early stages of the procedure, before the artificial tooth is placed over the implant.
What factors lead to the failure of dental implants?
Several factors can lead to the failure of a dental implant. These include:
1. Gum diseases
Healthy gums are a prerequisite and are evaluated prior to dental implant surgery. You cannot enter this procedure without first treating any disease, such as gingivitis or periodontitis.
Gum disease can damage the gums and jawbone. An uncontrolled infection could develop around the implant and cause it to fail.
2. Smoking
Smoking can also cause dental implant failure because it restricts blood flow to the gums, slowing down the healing process. Many research studies show that smokers have a higher rate of dental implant failure compared to non-smokers.
Being a smoker does not mean that you are prohibited from having a dental implant placed. However, you may have a better result if you stop smoking one week before dental implant surgery and if you do not smoke for at least two months after the implant is placed.
3. Insufficient jaw bone
A successful procedure also depends on having sufficient bone to support the implant. Without adequate minimum dimensions and healthy bone, the surgeon cannot surgically place the implant in your jaw.
4. Medical conditions that may lead to implant failure
Dental implant failure is possible if the patient is diagnosed with an autoimmune disease, advanced osteoporosis, or conditions such as gum disease, rheumatoid arthritis, and diabetes that slow down the body’s healing process. Slow healing can prevent osseointegration, and the implant does not integrate with the jawbone. If you have recently undergone chemotherapy or have had a serious heart attack, there may be a delay in healing. This is also true for people who smoke, drink alcohol and take medications for other diseases.
The use of certain medications (most commonly osteoporosis treatments) can also lead to failure of dental implants. Therefore, it is important to tell your surgeon about any prescription and over-the-counter medications you are taking.
You should properly inform your dentist of any pre-existing condition during a medical history review.
Complications from bisphosphonate medications
Bisphosphonates are a class of medications taken for bone loss or osteoporosis. The most common bisphosphonate medications are Fosamax, Actonel, Boniva, Bonefos, Bondronat and Reclast.
Bisphosphonates are used to reduce bone events in patients with osteoporosis, in patients who have been receiving anti-cancer therapy for a long time, and in patients with bone disease.
Extensive scientific research on dental implant complications from bisphosphonates shows that Fosamax causes the greatest risk of developing osteonecrosis of the jaw, which is a very serious bone disease.
Osteonecrosis of the jaw is a rare, but potentially serious complication of treatment with bisphosphonates and/or denosumab. It is important that dentists know how to diagnose and treat patients who are at risk of developing this complication.
The risk is small and is not always a deterrent to implant placement. However, you should tell your dentist if you are taking a bisphosphonate to prevent osteoporosis or as a cancer drug and he or she will decide if and how you can proceed with implants.
Problems due to bone loss
Failure at both early and later stages can also occur when there are not the minimum bone dimensions needed to support a dental implant. The most common reason for insufficient bone to have an immediate and successful implant placement is when a long period of time has elapsed between the loss of the natural tooth and the time of restoration with a dental implant. When the roots of the natural teeth are not present, the jawbone atrophies. Gum disease, such as periodontitis, also leads to bone loss. To restore with dental implants in such cases, special regeneration techniques are used which require a highly experienced and highly skilled dental team. Often, due to the technical difficulties of the regeneration techniques or incorrect surgical approach, the required steps are not taken and the dental implant ends up in an incorrect, prosthetic, position or is not surrounded by at least 1.5-2mm of healthy bone. Failure in such cases is predestined, sooner or later problems appear. In most cases the implant surgeon can complete the procedure using special bone regeneration techniques. Without sufficient bone, the implant cannot integrate with the jawbone. Learn more about bone grafting in our Guide to Dental Implants.
5. Poor tooth care
Maintaining good oral hygiene after a dental implant also has an impact on the success rate. You should perform proper cleaning as you do with your natural teeth and visit your dentist regularly.
6. Not following your dentist’s instructions
Your activities and habits have an impact on the success of the implant. Not following your doctor’s instructions may lead to implant failure or complications. After surgery to reduce the risk of complications, you may be asked to eat soft foods until the implant area has healed, practice good oral hygiene and avoid hard foods such as candy.
Instructions will be simple, such as reducing physical activity and cleaning the oral cavity. You will also need to follow dietary restrictions and take your medicine as prescribed.
7. Choosing the right dentist
Not all dental surgeons have the necessary experience and training and there is a chance of dental implant failure if you are treated by an inexperienced surgeon. Your dentist may refer you to an oral surgeon, but you can also choose your own.
An experienced implant surgeon will plan your treatment in conjunction with a prosthodontic specialist dentist who will undertake the prosthetic restoration. The detailed analysis of each specific case and the complex special techniques that must be employed require a team of specialists today for long-term dental implant success. Good intentions, which most healthcare professionals certainly have when handling a passerby, are not enough.
It is important to find a reputable implant dentist who has gone through proper certification. These qualified dentists know very well how to apply the right procedures and instructions, depending on your overall health condition. This will minimize the risk of infection and other complications that lead to dental implant failure.
Also, working with an experienced surgeon can prevent iatrogenic problems, as the areas of the jaw where dental implants are placed are adjacent to sensitive anatomical elements such as nerves and blood vessels.
In other words, to avoid problems, choose an implant surgeon with years of experience and expertise working alongside a qualified Prosthodontist Dentist for high quality functional and aesthetic restoration.
Planning before the dental implant procedure
Proper planning by an implant surgeon requires the doctor to complete a thorough examination of your mouth to evaluate the health of your gums and jawbone.
Dental x-rays give your surgeon a picture of your overall oral health, providing clues as to whether a dental implant will succeed. A special CT scan (Cone Beam Dental CT Scan) of the area is also required for accurate treatment planning, which when done with special modern equipment has minimal radiation and high resolution.
The planning also includes a detailed analysis of your medical history. This includes any medical conditions you have, as well as any medications you are taking.
When there is a lack of understanding of potential complications or proper planning based on the patient’s needs, a surgeon may proceed with a dental implant even when the patient is not a suitable candidate for such treatment.
This can cause improper placement of the implant and premature pressure on the implant without the necessary specifications, resulting in the development of infections, abscesses or necrosis in the implant placement area. More than a few patients come to our clinic to correct such problems, especially after implant placement in neighboring countries that advertise “cheap” implants. Read our related article on the Cost of Dental Implants and you will understand why such cases occur.
Careful treatment planning is important. Your surgeon should identify problems that could affect an implant. For example, you may need sinus elevation or bone grafting prior to implant placement to ensure success.
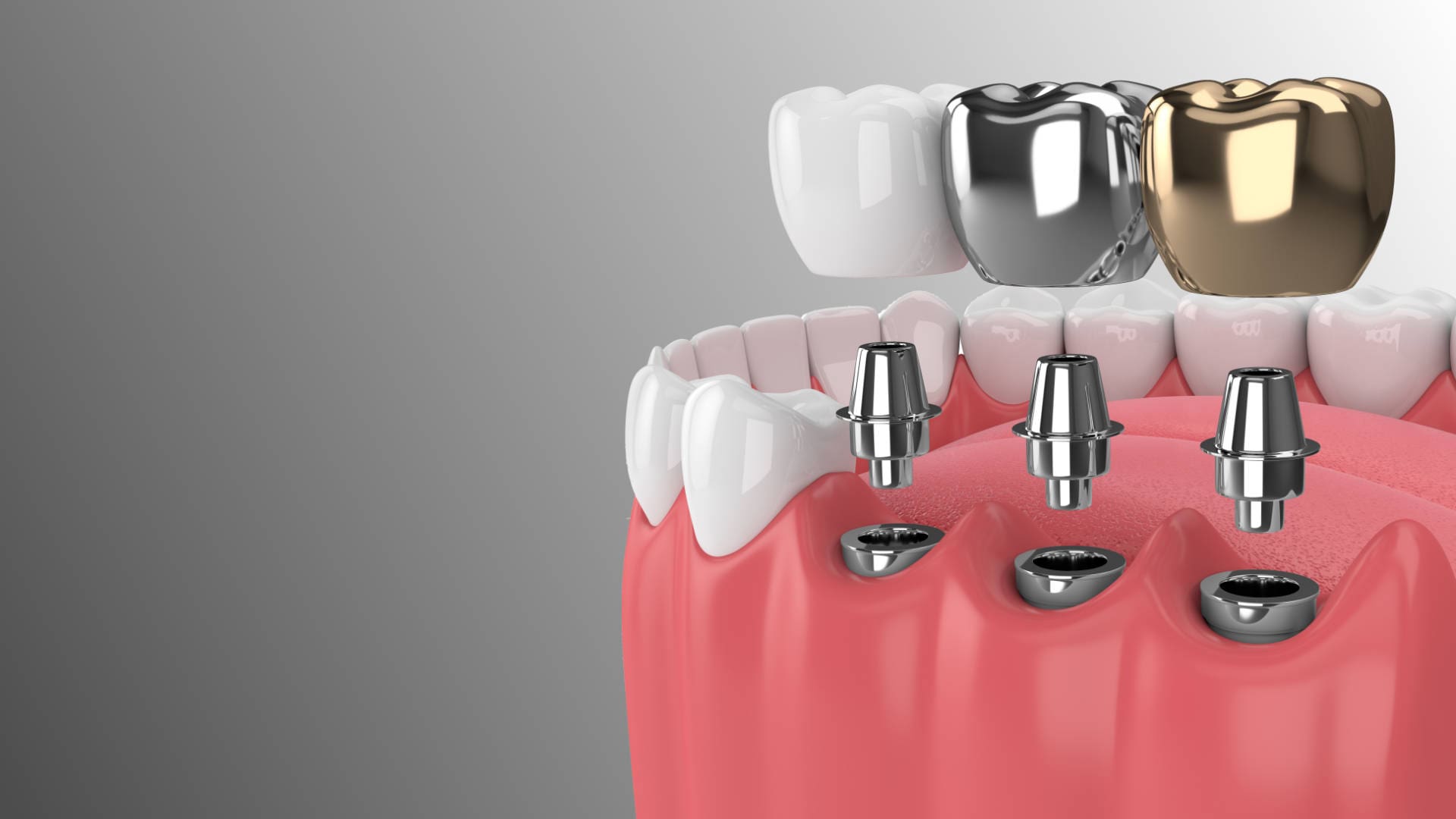
Successful implants occur when they integrate with the bone on all sides. If your bone is less dense or inadequate in any way, your dentist may need to perform additional steps to ensure that the bone has enough growth around the implant. If your tooth is missing for a long period of time, you could have bone volume loss. An experienced implant dentist can resolve this problem with bone grafts or another technique. Sometimes, this may be an additional necessary procedure.
Problems or complications after surgery
Implant complications can occur shortly after the procedure or many years later. Early implant failure occurs within the first three to four months after placement.
Also, keep in mind that you will experience some degree of pain or discomfort after surgery, which can be managed with simple pain medication. However, contact your surgeon if the pain does not improve after five to seven days.
While pain and swelling are common after surgery, pay attention to complications that may occur, such as:
Infection at the implantation site
An infection can develop during or after surgery. Your dentist will follow all aseptic and atraumatic techniques, minimizing the chances of infection during the procedure. However, the mouth is full of bacteria and there is always the possibility of an infection.
You can expect swelling, mild pain or discomfort for 1-4 days after the procedure. After this time, something may have gone wrong and you should consult your dentist.
Most issues related to infections and poor healing are the result of patients not following proper instructions after surgery. In rare cases, an infection develops after a month after surgery. In most cases, an underlying disease that was not detected before the procedure caused the infection.
If an infection or poor healing is detected early, it is treated accordingly and subsequent stages can continue successfully.
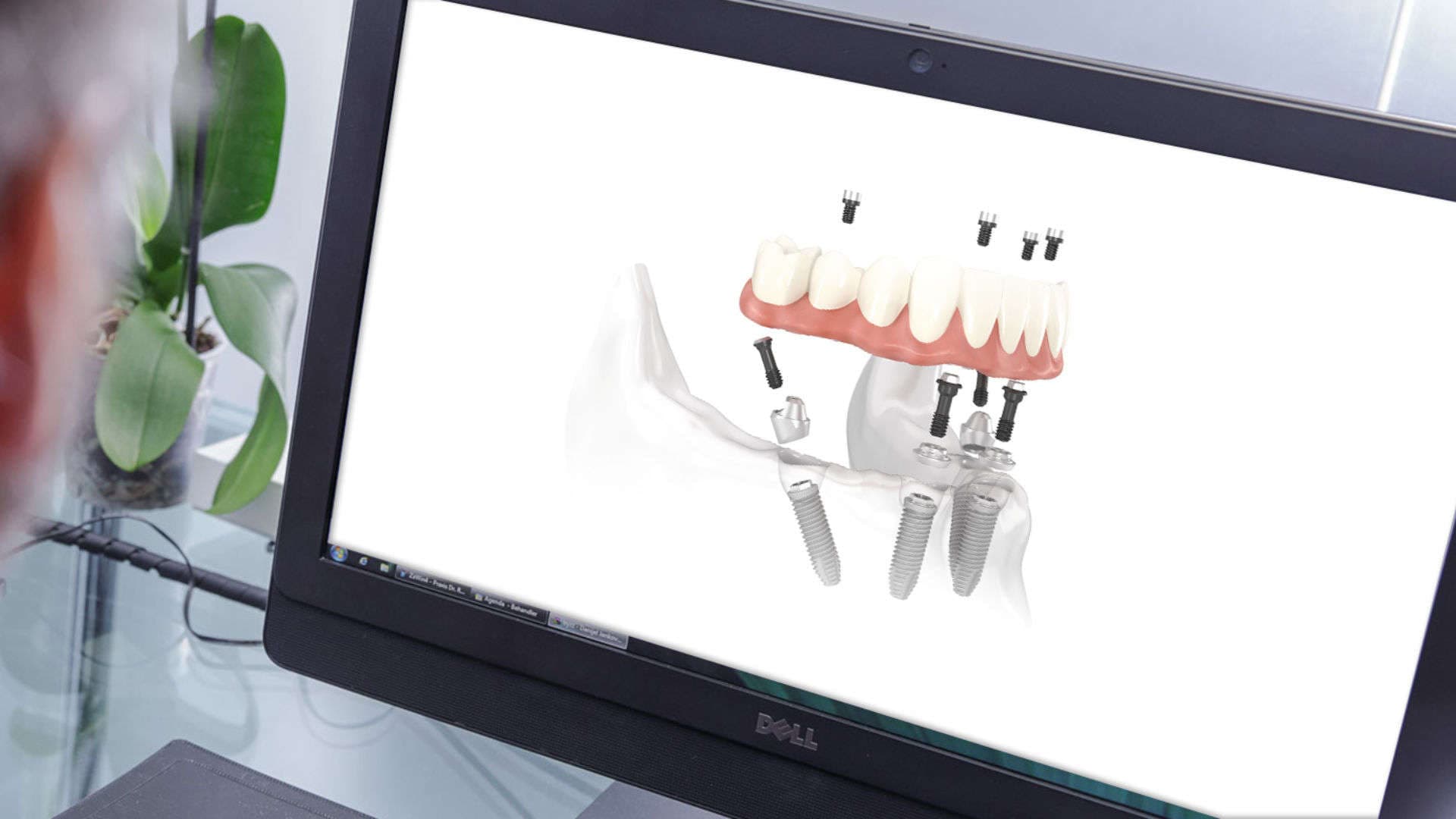
Implant mobility
Implant mobility can occur when a dental implant lacks stability. This can occur after immediate tooth replacement. Dental implants need to be immobile for a few weeks in order to complete the osseointegration process. Any movement that hinders this process will result in unstable implants. There are techniques where implants are directly supported by prosthetic work which are done when very specific conditions exist. These are highly specialized techniques that require an experienced implant surgeon and planning of the prosthetic work by a qualified prosthodontist.
During the first 2 – 12 weeks, the implant is vulnerable to the bone surrounding it not growing. This is very painful and you could end up back in surgery again.
Follow your dentist’s dietary recommendations after the procedure.
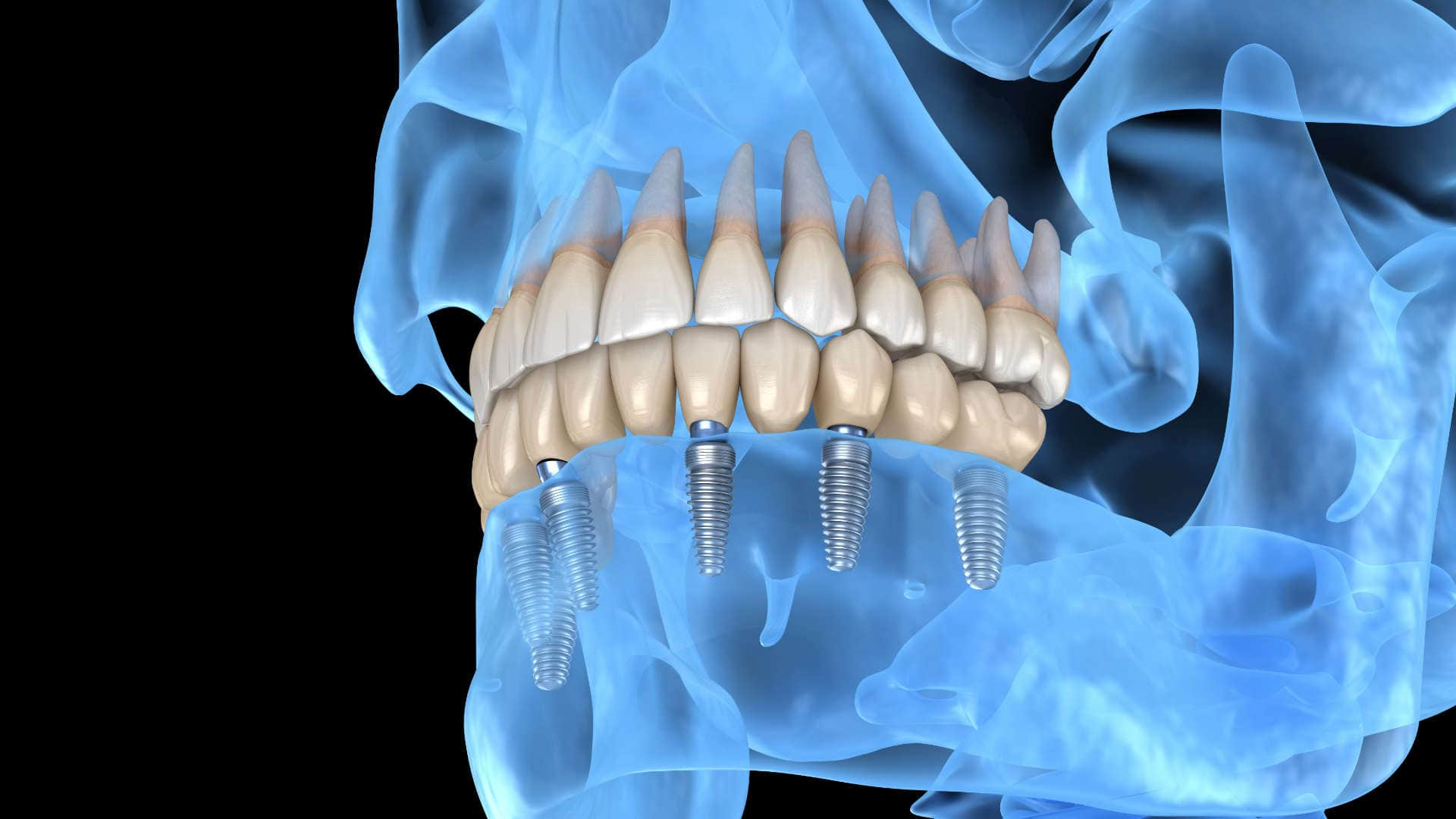
Usually, an artificial tooth is not attached to an implant until after it has been osseointegrated, with the exception of the All On 4 implant procedure. But sometimes, a surgeon performs immediate tooth replacement after implantation. This method requires fewer visits to the dentist, but it can also put extra pressure on the implant that has not yet fully integrated into the jawbone and lead to failure.
Implant failure and problems after years
Dental implant surgery can be an immediate success, but after a few years some complications may arise. Here are some such dental implant complications:
Nerve or tissue damage can occur when a surgeon places an implant too close to the nerve. Signs of damage include numbness or tingling in the tongue, lips, gums or face.
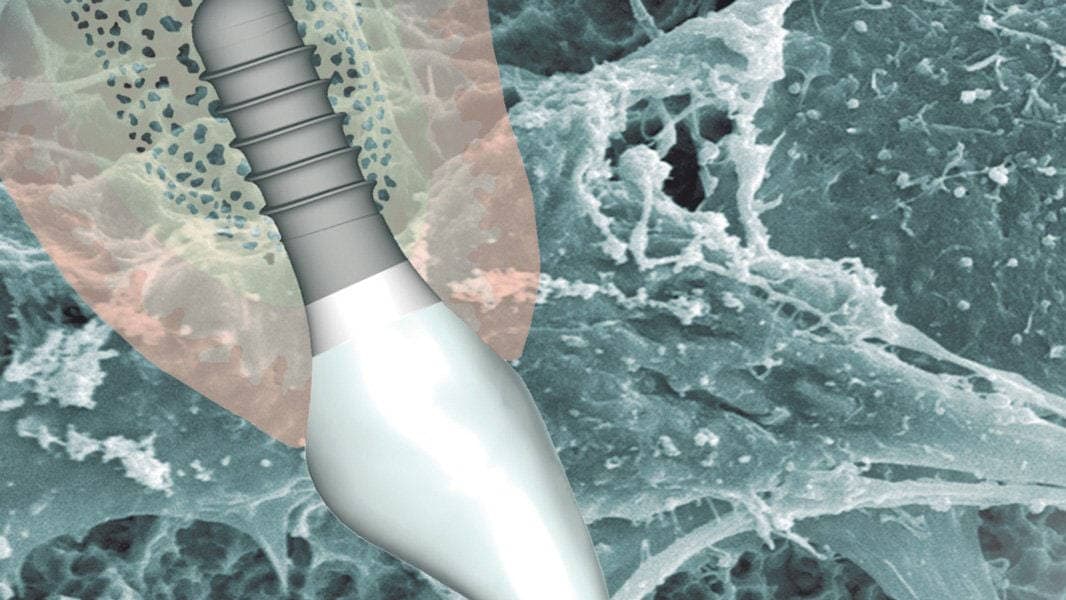
Foreign body rejection is rare, but it can happen. It happens when the body rejects an implant. That’s why we use titanium implants that are proven to be biocompatible with the human body. Read in our related article Which Are the Best Implants. Signs of rejection include increased pain at the implant site, swelling, fever and chills.
A dental implant placed in the upper jaw can protrude into the nasal cavity.
Injury to the area surrounding a dental implant can loosen the implant, resulting in failure.
Improper and absolute application of prosthetic work on the dental implant or the presence of tension in large prosthetic work leads, with mathematical certainty, to long-term implant failure. Sometimes even if the technical errors of an inexperienced and properly trained implant surgeon do not cause immediate problems, improper fabrication of the prosthetic work leads, in the long run, to implant restoration failure.
To minimize the risk of complications and prevent your implant from failing, continue to practice good oral hygiene to keep your mouth, implants and gums healthy. Brush and rinse your teeth at least twice a day, use mouthwash and visit your dentist regularly.
Signs of impending dental implant failure
Signs of a complication that may potentially herald dental implant failure include:
A common infection is peri-implantitis, which is a type of gum disease (equivalent to periodontitis). If left untreated, it can lead to serious complications such as bone loss or implant failure.
Signs of dental implant infection include:
- Difficulty chewing.
- Gum inflammation.
- Gum recession (receding) of the gums.
- Increased swelling – swelling in the implant area that persists.
- Mild bad taste/odor.
- Pus or bleeding of the gums in the implant area.
- Loosening or mobility of the prosthetic work.
- Severe pain or discomfort that is not controlled with simple painkillers.
- Persistent fever.
- Implant mobility.
If you notice signs of infection, call your dentist immediately.
Preventive care
Although some dental implant failures cannot be prevented, you can take steps to reduce the risk of failure:
- Properly care for your dental implants. Care for your dental implants properly.
- Visit the dentist every six months.
- Stop smoking. If you can’t stop, at least reduce it.
- Increase your calcium intake to have strong bones. Take a supplement or eat calcium-rich foods such as milk, yogurt, broccoli, oranges and cheese.
- Ask your dentist about a specialist in treating bruxism, in case you suffer from grinding or clenching of teeth.
Avoid eating habits that harm teeth, for example eating ice or candy or sugary foods.
Thorough preparation is the best prevention
Dental implants have high success rates, but they can fail for a number of reasons. It’s important to know the potential risks so you can take steps to reduce the chance of failure. This includes seeking treatment for gum or bone problems before surgery, choosing an experienced surgeon with the right expertise, and taking care to maintain good oral hygiene before and after surgery.
If you have problems with your implant
If you are experiencing problems with your dental implants, you need an experienced dentist who will be able to identify the importance and causes of the complications and know what treatment to follow depending on the problem. At Advanced Implant Clinics, our implant surgeons and prosthodontists will provide you with the high-quality care needed to treat the problems you may have. Contact us today to get the dental care you deserve.